Substance Abuse Can Affect All Ages
Though talk about substance abuse usually revolves around adults, young people are by no means immune to the impacts of addiction. Every year, 300,000 youth are arrested for drug- or alcohol-related offenses— which comprise 20% of all juvenile arrests across the U.S. But youth substance abuse expands beyond the juvenile justice community. In a 2017 nationwide survey of
Opioid Epidemic

After more than 10 years of rising death and abuse rates, there is little debate: The United States is facing a health crisis centered on the use of powerful opioids. About two-thirds of all overdose deaths in 2016 involved an opioid, and an astounding 115 Americans per day die after an overdose on these powerful drugs.3 But not all opioids are created equal. The word itself encapsulates three different types of drugs: prescription painkillers like OxyContin, heroin itself and synthetic opioids found in drugs like heroin and cocaine. Though different substances, these three categories are chemically linked by the effects they cause in the human brain—for many, this means that the abuse of one opioid can easily lead to the use of another. In fact, those who abuse prescription painkillers are over three times more likely to begin using heroin as compared to those who don’t.4
This is particularly dangerous for adolescents, who often begin opioid use with prescription painkillers like OxyContin or Percocet. In 2015, 276,000 juveniles used non-medical pain relievers, and of those, over 44% qualified as addicted to those pills. Many of these young people don’t have prescriptions
A jump in youth substance abuse rates isn’t the only way children are affected by the opioid crisis—with more and more adults abusing opioids, youth are at an increasingly higher risk of living in dangerous or neglectful households. From the very beginning of their lives, youth born to a mother with an opioid addiction can experience natal complications, like the inability to feed and developmental delays. The number of babies born addicted to opioids has increased fivefold in the past decade, another sign of the opioid crisis’ grip.5 Slightly older children also face risks of exposure to these drugs—the rate of youth admitted to hospitals after opioid overdose has doubled since 2004, many of these occurring after young children accidentally ingest their caretakers’ pills. And juveniles of all ages are affected by growing up in households with substance abuse issues— these youth are more likely to exhibit behavioral problems, struggle with mental health issues and abuse substances themselves in the future.6 From the youngest children to high schoolers, the opioid crisis has damaged families and the lives of juveniles.
Drug Courts
For youth that
Many sentences in juvenile drug courts include mandatory drug testing, an aspect of treatment that is meant to keep youth accountable but can lead to further penalties if broken. While drug courts generally refer youth with substance abuse problems to treatment centers, courts rely on routine drug screenings to ensure that young people are maintaining their commitment to therapy. But drug testing as a means of accountability without a therapeutic approach can be problematic. This method can be inaccurate, sometimes incentivizing juveniles to “cheat” on their drug tests rather than focus on recovery. What’s more, being tested by a professional can cause mistrust or a superficial relationship between a therapist and an adolescent, leading to a lack of meaningful conversation about substance abuse. If youth are found failing a drug test, they can be resentenced to longer or more onerous punishments, even including detention. Juvenile drug courts are historically under-researched, but recent studies have found mixed results of these courts on juvenile recidivism rates and future substance abuse.7
Reflecting a national trend towards evidenced-based, individualized therapy for youth, the Office of Juvenile Justice and Delinquency Prevention (OJJDP) recently released new guidelines for juvenile drug courts that emphasize family and community engagement. Taking the focus off screenings, the OJJDP created a list of new tasks for drug courts: include local schools and communities in the treatment process, provide options for non-English speakers, assess the needs of parents—including parental mental health treatment—and support youth with evidenced-based treatment options. The OJJDP urged drug courts to move away from the use of fees and detention, and to instead focus on creating healthy support networks for juveniles—this reform trend is becoming popular in all areas of the juvenile justice system.
Substance Abuse and Mental Health

For both adults and children, substance abuse issues oftentimes come along with or even cause mental health complications. Called co-occurring disorders, substance abuse
Youth in the juvenile justice community tend to have higher rates of co-occurring disorders than their counterparts. Studies show that mental health issues are overrepresented among youth in the system, with some jurisdictions reporting that up to 70% of entrants have been previously diagnosed.9 The longer that young people spend in the system—often moving from probation to detention—the more prevalent mental illness in this population becomes. Substance abuse is also more common among youth in the juvenile justice system, with some estimates of disorder rates reaching as high as 60% of all entrants. As compared to youth outside the system, adolescent offenders tend to have experienced more childhood trauma, higher rates of family poverty and challenges at school—this may explain why these young people demonstrate higher rates of co-occurring disorders. But youth suffering from a mental or substance abuse disorder are more vulnerable to exploitation and other adverse consequences while in detention; it’s imperative that juvenile courts provide other options.
Juvenile justice reformers are increasingly focusing on substance abuse and mental health treatment as important, cost-effective alternatives for youth. In light of research demonstrating that putting vulnerable youth in greater contact with the juvenile justice system can be harmful to their recovery, reformers are advocating for a heavier emphasis on treatment regimens separate from the court system. Rather than refer youth to multiple different service providers—one program for mental health, and another for substance abuse support—reformers are now recognizing the need to simplify treatment for adolescents. Using one regimen that provides comprehensive, multilateral treatment for co-occurring disorders can be a much more powerful and effective experience for juveniles—the push to fund and implement these programs countrywide is underway.
Treating Youth Substance Abuse
Researchers and reformers alike know that threats of punishment and detention are ineffective when treating substance abuse among youth—programs that involve family, school and community engagement, with emphasis on positive development, have seen higher success and lower recidivism rates. Substance abuse treatment can be split into a few different categories—behavioral interventions are more “traditional” therapy, in which juveniles travel to facilities or live in centers to receive treatment. Therapists may provide incentives to remain sober, coach youth in life skills and suggest strategies for coping with temptations in different environments. Some behavioral interventions can take place in group therapy or group homes, though these ecosystems carry the risk of sparking conversations that glorify drug use, undermining the recovery process. The juvenile justice system is now tilting away from these types of therapies and towards family-based approaches, the most successful and cost-effective substance abuse intervention for youth.
Family-based approaches are treatments that highlight full family engagement in the recovery process, from caretakers to siblings. These interventions often address co-occurring mental health disorders as well, and they generally offer services for caretakers as well as the young person. Multisystemic Therapy (MST) is one of these family-based approaches. MST is a research-based, comprehensive outpatient substance abuse treatment that considers the family as the heart of support for a young person. That’s why MST works with not only youth but also caretakers and siblings, offering services like parental skills training, career planning
Multisystemic Therapy and similar family-based approaches are so efficacious because they are well-equipped to address the complex, often intertwined issues of substance abuse and mental health issues. MST therapists help families and youth set goals together, leaving accountability with caretakers rather than courts and helping young people transition out of the juvenile justice system. Juveniles complete MST treatment more often than group homes or traditional therapy, with completion rates worldwide at over 85%. Compared to usual services, MST youth are less likely to face rearrests for drug-related offenses and report lower rates of drug use after treatment—in fact, after implementing MST in Connecticut, 98% of juveniles had no new drug-related arrests during treatment. Research like this demonstrates why the juvenile justice system is increasingly engaging with home- and family-based approaches—with more treatment systems that engage families and communities, youth with complex substance abuse disorders have a higher chance of quick reintegration and recovery.
Juvenile Justice Reform-Video
A part of juvenile justice reform is finding new ways to help at-risk youth with better outcomes. Judge Teske has the option of sending youth to detention centers or placing them in programs like MST. MST works with families to affect positive change. Caregivers learn how to hold their children accountable for their behavior. Judge Teske talks about how MST's teen crime therapy can stop crime and reduce the number of incarcerated youth. Watch this short video. Click here to watch Judge Teske's full video.
U.S. Department of Health and Human Services
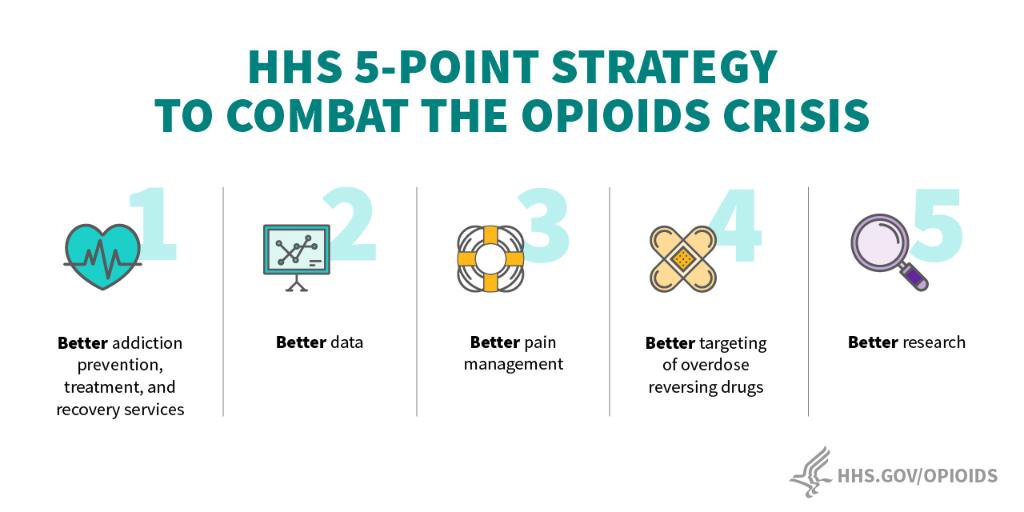
Funding Youth Substance Abuse Programs
The MST approach to putting juvenile offenders on the right path has been shown to be extremely effective in terms of its success rate, decrease in crime and keeping down costs. The question becomes how can communities and organizations pay for MST programs? Here are four steps that should be considered:
-
Assess whether your community needs an MST program.
-
Determine what funding is available.
-
Set up sustainable funding that will be in place for years.
-
Focus on long-term strategies.

Contact Us
Interested in starting an MST program in your area?
Fill out the form below and someone will contact you shortly.